
The relactation process
Relactation is the re-establishment of breastmilk supply in a woman who has given birth, after milk secretion has significantly been reduced, interrupted or inhibited altogether, either because of inability or unwillingness to breastfeed after childbirth.
Requests for help in relactation are common, it is a process in which women must be accompanied and they need to know very well the steps and actions to be taken to increase breast milk production while reducing the amount of formula offered to the infant. This is a gradual process and, unless the daily intake of formula milk is equal to or less than 100ml (3.38oz), it is not advisable to do it abruptly.
In relactation, two factors directly affect the chances of success: the infant’s willingness to suckle and the mother’s ability to increase milk supply. Finally, the decrease in the amount of formula milk given should be done gradually.
Assessing the infant’s willingness to breastfeed
It is essential to assess the infant’s willingness to breastfeed, which means evaluating if she or he is interested in feeding directly at the breast. The following figure can also help in decision making:
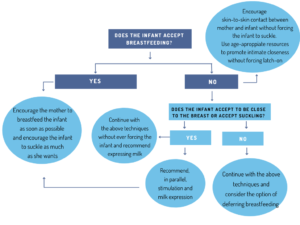
Whether the infant accepts to suckle or the mother wants to keep trying to get the baby to latch onto the breast, it would be ideal to recommend pumping to increase stimulation and milk expression, which should lead to an increase in milk supply.
Increasing the mother’s milk production
To increase milk production we can encourage the mother to offer the breast whenever the infant is willing to suckle, ideally 8-12 times in 24 hours. As the baby is suckling, breast compressions can be used to facilitate a steady flow of milk and reduce the risk of the infant getting tired or refusing the breast.
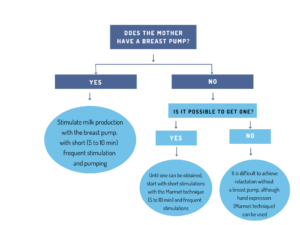
At this point, it is essential that we assess together with the mother, how often she will be able to pump. It is key, that she can see a reachable goal, as recommending excessive pumping can be discouraging. Therefore, a general guideline is to use a breast pump throughout the day (after feeding or 1 hour after feeding) as many times as she wants and is able to do so, but for a short time: 5-10 minutes each time is more than enough. Frequent and brief pumping has been shown to be more effective than prolonged and occasional use.
Reducing formula or breastmilk supplementation
When deciding to start reducing milk supplementation, it is essential that the underlying cause that led to supplementation has been resolved. It is also recommended to make sure that the infant is at an appropriate weight for his or her size and age.
First, measure the amount of supplemented milk the infant takes in 24h. If this is not known, we recommend monitoring for a few days to see how much milk supplementation the infant usually has. This way we will be able to know the amount of supplementation we are starting from, so we can begin to reduce it.
Usually, as long as there is no problem of hypogalactia or difficulty in milk transfer, it is recommended to gradually reduce approximately 60ml of supplemented milk every 2-3 days, but each case needs to be assessed on an individual basis.
There are several options to reduce:
- Eliminate 60ml (2.03oz) from a single feed. It is often easier to do so in the morning feeds when the baby is generally calmer.
- Decrease 10ml (0.34oz) of supplemented milk in 6 feeds
- Decrease 30ml (1.01oz) of supplemented milk from 2 feeds
After two or three days of eliminating this amount of milk, it is key to talk to the mother and evaluate how she is feeling during the process. If the infant is not overly demanding, if there are no warning signs that she/he is not getting enough milk and the mother feels well during the process, another 60ml (2.03oz) can be eliminated again in the same way.
It is essential to monitor adequate weight gain, but do bear in mind that it is not recommended to weigh the infant before 5-8 days of age. It is also important to inform the mother of the possibility of the baby being more demanding, as well as to explain the signs and symptoms of dehydration (assessment of diuresis and stools, as well as the baby’s general condition).
More aspects to consider about relactation:
The above guidelines are the basis of the process, but you can also encourage the mother to perform small actions, which can favour the relactation process:
- Assess together with the mother, whether the use of a galactagogue may be appropriate. Its use may encourage increased milk supply and thus encourage both, mother and infant, to continue the relactation process.
- Encourage the mother to cosleep with her baby (by giving advice on how to do so safely), as it is usually easier for the infant to accept breastfeeding during the night when prolactin levels peak and therefore favour the relactation process.
- Encourage the mother to offer supplemented milk in a breastfeeding-friendly way. If a bottle is used, inform the mother about the paced bottle feeding method.
- Eliminate the use of pacifiers (dummies) as much as possible, to encourage infants to calm their suckling needs directly at the breast.
References:
. Hormann, E., Savage, F.. Relactation. Review of experience and recommendation for practice. Child and adolescent health and development. 1998; 14: 1-30. Available at: https://apps.who.int/iris/bitstream/handle/10665/65020/WHO_CHS_CAH_98.14.pdf?sequence=1. 27/02/2021.
. Lawrence, Ruth A.; Lawrence, Robert M. Breastfeeding. A guide for the medical profession. Seventh Edition. Missouri: Elsevier Mosby; 2011.