Relactation: process and stages
Relactation is the process of restoring a mother’s breast milk supply after it has decreased or disappeared altogether. For various reasons, mothers may wish to stop supplementing the artificial formula they give their infants and attempt to resume exclusive breastfeeding.
Correcting the cause of relactation
Before starting with the relactation process, the causes that led to the initiation of supplementing formula must be investigated as in some situations, it will be very unlikely that relactation can be achieved. These situations are:
- Breast hypoplasia
- Mastopexy
- Certain medications may interfere with both lactogenesis II and galactopoiesis.
- Presence of the underlying problem that caused the need for relactation (complicated ankyloglossia, lingual hypotonia, etc).
In these cases the pros and cons of starting this complex process must be assessed with the mother, taking into account that the success of the process is compromised by these issues.
The challenge in relactation is to increase the mother’s milk supply while decreasing the amount of commercial formula milk the infant takes. Therefore, before starting the process, it is recommended to instruct the mother to keep a record of the amount of formula she gives the baby for a couple of days. Many mothers are not fully aware of the volume of formula they give in 24 hours to their infant. This is a key point, as when starting a relactation, it is not possible to completely eliminate formula supplementing if the infant has more than 100 ml of formula per day.
Usually, the quantities are much higher than 100 ml, so in these cases, a gradual relactation process must be scheduled and followed, so milk supply can normalize with adequate stimulation of the mammary gland.
This process can be slow and needs support from healthcare professionals and the mother’s family.
Basics for initiating relactation:
- First of all, try to verify what went wrong and why supplementing has been necessary: make an exhaustive evaluation of a feed at the breast, the mothers’s breasts, the baby’s sucking rhythms, the existence or not of tongue-tie or retrognathia as well as any other orofacial deformation, check thyroid values and so on. In this way, you can ensure that no limitation interferes with achieving a relactation.
- Babies usually present a more correct sucking pattern when they are still in a phase of sleepiness, don’t wait until they are too active to put them to the breast. If the baby refuses the breast, the best thing to do is not to force them and not to bring them closer to the breast.
- Skin-to-skin contact and the so-called “seduction” techniques are very useful for the baby to feel comfortable near the breast, it should be their choice to breastfeed and not an obligation.
- Encourage the mother to offer the breast at least every two hours during the day, every three hours at night or whenever the baby is ready to breastfeed.
- Propose safe co-sleeping as a form of rest and as a way to facilitate nighttime feeds.
- Ideally, eliminate pacifiers and bottle teats so that the baby can focus solely on sucking from the breast. Since formula will need to be offered, look for other feeding methods that avoid nipple confusion and the extreme satiety that bottle feeding can produce.
- The first few days of trying to increase milk supply, and if the baby is mostly on formula, continue giving the full amount of formula recommended for the age and begin to stimulate the breast with a breast pump.
- It is advisable to feed the milk (expressed breast milk or formula) to the infant with a non-invasive supplementing method.
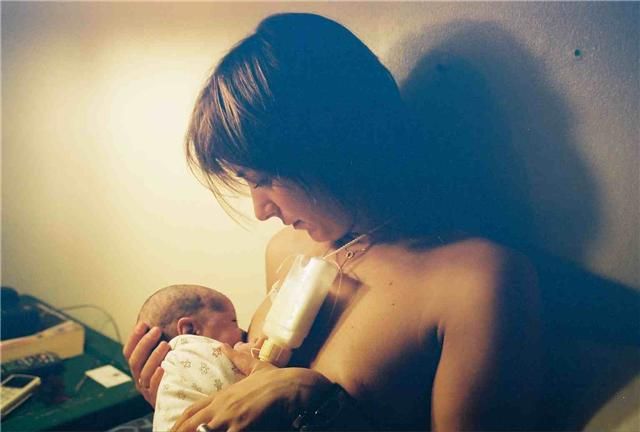
- In the event that the baby presents nipple-teat confusion and is frustrated when suckling, crying, irritable, or does not suckle for long periods of time, the use of a supplemental nursing system( SNS) may be considered.
- To ensure that the infant gets enough milk, pay attention to the baby’s weight gain (30 grams per day for the first 6 weeks) and 5-6 wet diapers per day with clear urine. However, some babies, when starting relactation, may show a temporary stagnation in their weight development, even a slight weight loss.
- If the baby is not getting enough breast milk and is not gaining weight properly or is fussy and restless, do not reduce the amount of formula for a few days and, if necessary, increase the amount of formula again for a day or two.
To increase breast milk supply:
- The mother should begin stimulating the breast with a breast pump and, if possible, finish by hand expressing breastmilk manually, as this provides better stimulation and more milk volume.
- Recommend the mother to keep expressing breast milk as many times as possible throughout the day. Only a few minutes are needed each time during the first weeks.
- The minutes of pumping will increase together with the achieved amount of milk.
- Always pump at dusk and at dawn to take advantage of the higher prolactin levels.
- Consider prescribing the mother a galactagogue if she does not see satisfactory progress in the amount of breast milk obtained.
A useful way to reduce formula milk supplementing when breast milk supply has increased is as follows:
- Reduce the amount of formula supplementing given in 24 hours: 60 ml in total are eliminated. This reduction is maintained for a few days. This amount can be divided among several feeds: for example, reduce 10 ml in five formula feeds or reduce two feeds by 30 ml each.
- Continue with the reduced amount of formula for the following days. If the baby shows through their behavior that they are satisfied and if, after one week, has gained 125 grams or more in weight, reduce the formula supplementing again by the same amount for a few days and recheck the weight.
- If the baby shows signs of hunger or has not gained enough weight at the end of one week, do not reduce formula supplementing and continue with the same amount for another week. If the baby continues to show signs of hunger or still has not gained weight after another week, increase the formula back to what it was before the reduction.
- There are several patterns for formula supplementing and each mother chooses the one that works best for her. Some mothers prefer supplementing with formula only at a few feeds. Another common pattern is to only breastfeed the first few hours of the day and in the evening when the breasts feel softer and the babies seem more uncomfortable, give the supplemental formula milk. It is also possible to supplement only at some feeds.
Relactation is a long process that can take weeks of work, and it is very important for mothers to have the support of healthcare professionals to clarify any questions that may arise, assess the baby’s evolution, and strengthen their efforts. It should be taken into account that a relactation can not always be achieved and that the mother must be accompanied in the process when she does not succeed.
References
- Cevik, E., & Yasar, O. (2023). Interruption of Breastfeeding, Relactation, Relactation Awareness, and Related Factors: A Cross-Sectional Study. Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine, 18(1), 48–58. https://doi.org/10.1089/bfm.2022.0199
- Lommen, A., Brown, B., & Hollist, D. (2015). Experiential Perceptions of Relactation: A Phenomenological Study. Journal of human lactation : official journal of International Lactation Consultant Association, 31(3), 498–503. https://doi.org/10.1177/0890334415581646
- Muresan M. (2011). Successful relactation–a case history. Breastfeeding medicine : the official journal of the Academy of Breastfeeding Medicine, 6(4), 233–239. https://doi.org/10.1089/bfm.2010.0062