
Hypogalactia: How to Identify it and how to Accompany it?
Hypogalactia is defined as insufficient milk supply to maintain exclusive breastfeeding. A woman may have milk secretion, but this may not be sufficient, and she may need supplementation for the correct feeding of the infant.
Studies indicate that 36% of mothers attribute the end of breastfeeding to a lack of milk supply. In reality, in the majority of cases, this is only a perception and is not confirmed, but genuine hypogalactia exists in 5% of mothers either due to anatomical variations of the mammary gland or medical illnesses.
Hypogalactia can be a multifactorial process, it can be caused by one cause, or there can be several aspects involved that also revert back to each other and can cause a more pronounced drop in breastmilk production. Below is a list of possible causes that may occur alone or together:
- the baby is not drinking enough milk
- Infant’s incapacitating illness
- Premature infant
- Lack of access to the breast (restriction due to scheduled feeding)
- Poor milk transfer (e.g. ankyloglossia, suckling difficulties, etc.)
- Maternal pathology:
– Preglandular:
1. Retention of placental debris
2. Congenital prolactin deficiency
3. Sheehan’s syndrome / Acute anaemia (haemoglobin <10 g/dl)
4. Polycystic ovarian syndrome (POS)
5. Oral contraceptives
6. Medication
7. Social drugs
8. Transient hypogalactia (insulin-dependent diabetes, corticosteroid treatment, obesity) delayed onset of lactogenesis II.
– Glandular
1. primary hypoplasia, which is congenital
2. Secondary hypoplasia: due to mammoplasty or radiotherapy
– Postglandular:
1. Lactation technique
2. Separation of mother and child, routines (scheduled feeding), interference
3. Ineffective emptying of the breast
A proper diagnostic process with a mother-baby dyad suspected of suffering from hypogalactia should be carried out.
Suspicion of hypogalactia may be given by the following signs:
– Infant irritable at the breast, crying a lot.
– Infant who does not seem to stay full, who sleeps little, long feeds
– Mother with a feeling of empty breasts
These are all perceptions that should be investigated in more detail during the breastfeeding consultation.
Identification of hypogalactia
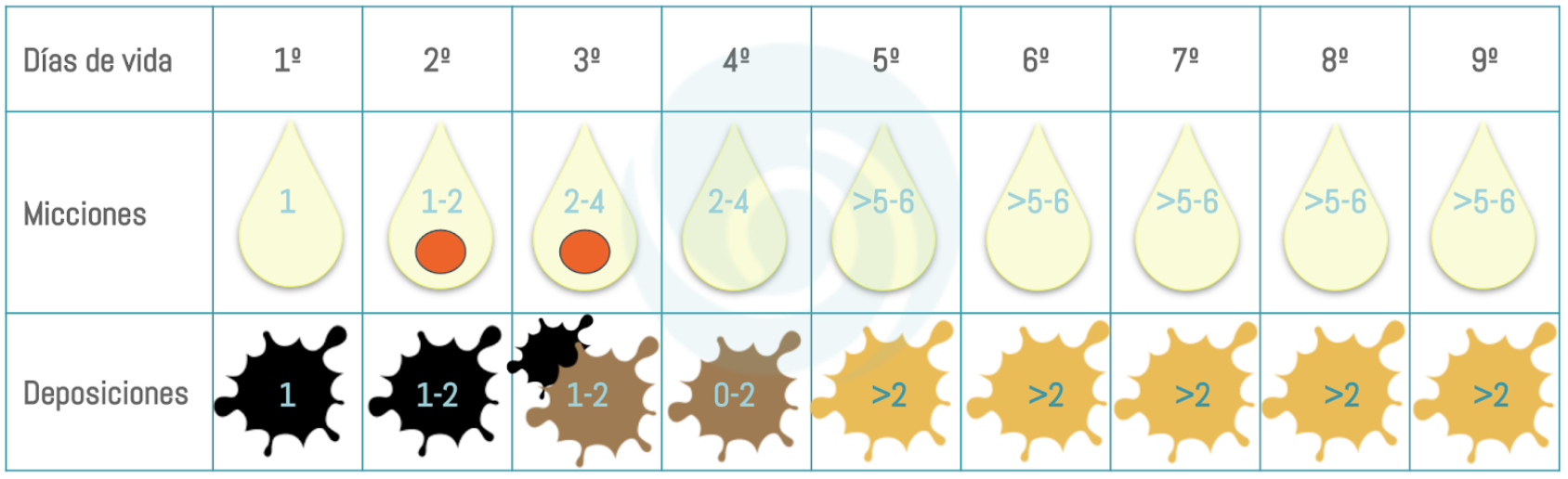
The first step should be to check the evolution of the baby’s weight, to check whether the baby has regained the birth weight, how quickly, whether the weekly weight gain is adequate or not, and so on. This step should be complemented with a follow-up of the infant’s stools, as sometimes, with a correct weight or within the lower limits, the key to revealing hypogalactia can be indicated with this data.
Once the baby’s weight has been checked, it is necessary to discuss with the mother whether she has noticed any changes in her breast tissue during pregnancy and in the immediate postpartum period; thanks to this information, it will be possible to determine whether there is a cause of hypogalactia due to a possible mother’s pathology. This should be investigated if the response indicates it and the above-mentioned differential can be followed.
Finally, among the three essential steps in consultations of this type, it is necessary to assess a complete feeding process at the breast, check if the milk transfer is correct, see how the baby behaves when the breast is brought close, and thus assess if there is any factor dependent on the baby that may lead to a low stimulation of the mammary gland, which results in low milk production.
The resolution of the problem will obviously depend on the cause. In some situations, it may be possible to correct the problem, such as an incorrect breastfeeding technique or a change in medication that might have reduced production. In other situations, it is necessary to help the mammary gland to be stimulated to increase production, for example, by adding extra breastmilk extractions with a breast pump or suggesting that the mother takes a galactagogue. In other situations, the infant needs to receive supplemental milk, especially if there are signs of dehydration or low weight gain. In these cases, it is necessary to assess with the mother which supplementation method is most appropriate for her situation and to explain the options available to her in relation to feeding her child.
References
-
Ramiro González MD, Ortiz Marrón H, Arana Cañedo-Argüelles C, et al. Prevalencia de la lactancia materna y factores asociados con el inicio y la duración de la lactancia materna exclusiva en la Comunidad de Madrid entre los participantes en el estudio ELOIN. An Pediatr (Barc). 2018;89(1):32-43. doi:10.1016/j.anpedi.2017.09.002
-
Lawrence, Ruth A.; Lawrence, Robert M. Lactancia materna. Una guía para la profesión médica. Séptima edición. Missouri: Elsevier Mosby; 2011.
-
Walker, Marsha. Manejo de la lactancia materna para el clínico. Using Evidence. 4rth Edition. Burlington, MA: Jones & Bartlett Learning; 2017.