Breastfeeding versus pathologic hyperbilirubinemia
Hyperbilirubinemia is a common situation in newborns. The shift from fetal hemoglobin to extrauterine hemoglobin causes increased red blood cell destruction, which will cause bilirubin values to increase, even more so if the bilirubin excretory system is not in its best condition.
Hyperbilirubinemia is described as a blood bilirubin concentration above 1.2 mg/dl.
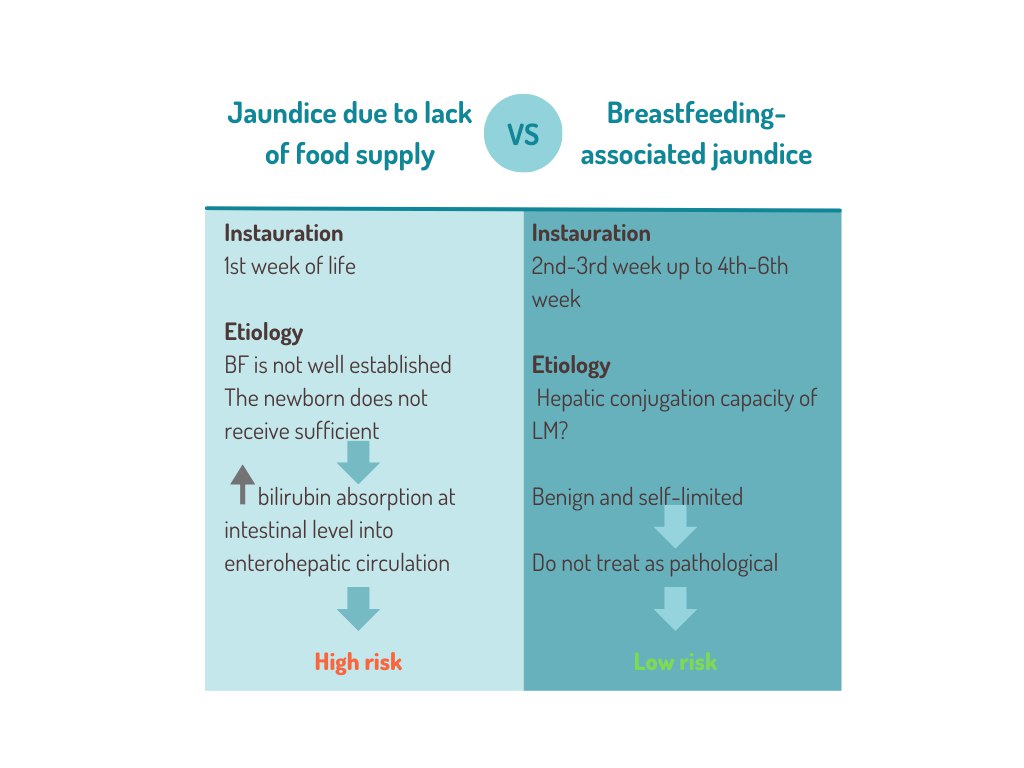
The etiology of hyperbilirubinemia in newborns can be multiple. However, in the field of lactation, two of these are relevant. The first is hyperbilirubinemia which occurs due to a lack of milk transfer, and the second is physiological and should not be treated.
The determination of bilirubin in the blood, with non-invasive methods, is necessary to avoid the complications of severe hyperbilirubinemia.
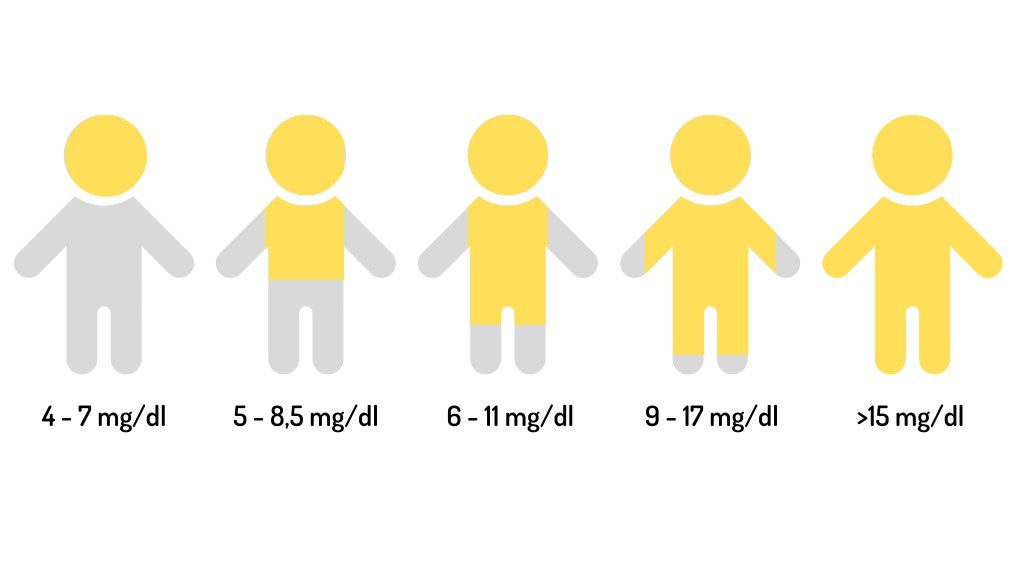
Although many units now have a transcutaneous bilirubinometer, it may still be useful to make use of the observational method, the so-called Kramer Zones, which relate icteric body parts to bilirubin levels in the blood:
This graph gives a quick idea of the situation and therefore helps to determine the need for complementary tests.
The main way of bilirubin excretion is through the digestive system. Most of it will pass into the small intestine through the biliary tract. A small proportion will be excreted in the urine. In the colon, bilirubin will be converted to urobilinogen. There is usually a small reabsorption of this component in the colon, passing into the blood again.
The remaining urobilinogen in the intestine will finally be excreted in the form of stercholine, which gives the typical color of the feces.
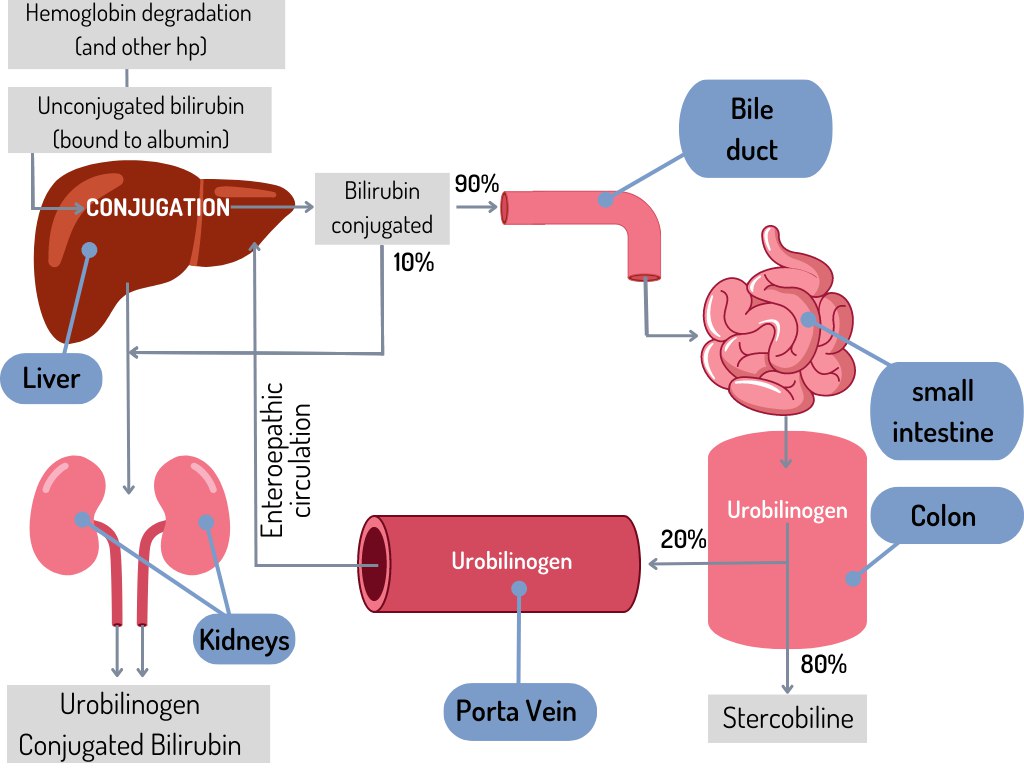
When there are difficulties in milk transfer (or hypogalactia) and the newborn does not receive enough milk, urobilinogen reabsorption is increased and thus decreases the success of digestive secretion. This increases blood bilirubin levels and creates a favorable environment for hyperbilirubinemia.
In these circumstances, it is important to note the reason for poor milk transfer. If the infant is exclusively breastfed, an exploration of the optimal establishment of breastfeeding should be done, looking for both maternal and neonatal causes.
Restoration of milk flow will improve the clinical picture. In severe cases, support therapies, such as phototherapy, will be necessary. Even so, it is important to remember that the main treatment will be the correct establishment of lactation.
A number of infants present with what is called breastfeeding-associated jaundice. This is a completely benign condition of little-known etiology, in which, from the second week of life, bilirubin values increase in the blood.
It is assumed that, in some cases, human milk inhibits the hepatic conjugation capacity of bilirubin. This is caused by the presence of a substance (β glucuronidase) in human milk, which is an antioxidant factor believed to make neonatal jaundice last longer, sometimes a month. However, in these cases, it is not necessary to treat the newborn.
References
R. Fernández Lorenzo, M. Couce Pico, J. M. Fraga Bermúdez. (2008). Hipoglicemia neonatal. Protocolos diagnósticos terapéuticos AEP, 18.
Wight, N., Marinelli, K. A., & Academy of Breastfeeding Medicine. (2014). ABM clinical protocol #1: guidelines for blood glucose monitoring and treatment of hypoglycemia in term and late-preterm neonates, revised 2014. Breastfeeding Medicine: The Official Journal of the Academy of Breastfeeding Medicine, 9(4), 173–179. https://doi.org/10.1089/bfm.2014.9986
Page-Goertz, S. (2010). Hypoglycemia in the Breastfeeding Newborn. En International Lactation Consultant Association (Ed.), Independent Study Module.
Bahr, T. M., Henry, E., Christensen, R. D., Minton, S. D., & Bhutani, V. K. (2021). A New Hour-Specific Serum Bilirubin Nomogram for Neonates ≥35 Weeks of Gestation. The Journal of Pediatrics, 236, 28–33.e1. https://doi.org/10.1016/j.jpeds.2021.05.039
American Academy of Pediatrics Subcommittee on Hyperbilirubinemia (2004). Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics, 114(1), 297–316. https://doi.org/10.1542/peds.114.1.297